Communication Skills: Explaining Cystic Fibrosis
Cystic Fibrosis is a complex multi-system disease which is usually managed by respiratory physicians due to its significant lung involvement. In an OSCE setting, the disease could be covered in many different types of stations in both general medicine and paediatrics. It is important to know the basics of the disease and to try to consider a few of the important questions which could be asked by any patient or relative.
We have included the main points below it is important to tailor your answers to the main concerns of the patient or relative. These could be, for example, around how the disease is caused, what complications it might produce, or what the treatments involve.
- Cystic fibrosis is an autosomal recessive genetic condition, which means that it is inherited through genes but frequently parents of an affected children can carry the gene without having the disease itself
- In the UK it occurs in approximately 1 in 2500 live births
- It is characterised by a defect on chromosome 7 (in 75% of the time this is due to a DF508 mutation however hundreds of mutations have been identified)
- This defects encodes the CFTR (CF transmembrane conductance regulator) chloride channel. This channel plays a vital role in secretory function in all exocrine tissues including the nasal epithelium, the lungs, salivary glands, pancreas, intestines and bile duct.
Defective CFTR protein prevents chloride from moving out of cells

Sodium is then absorbed to maintain electrochemical balance

Water follows sodium into cells by osmosis

This results in extracellular dehydration and thick, viscous secretions

These secretions are easily amenable to infection and chronic colonisation
Cystic fibrosis may be detected at birth, in the neonate, in early childhood or rarely in adulthood depending on the clinical presentation and severity.
Presentations can be grouped by systems as follows:
- H influenza and staph aureus (often in childhood)
- Pseudomonas
- Burkholderia cepacia this is associated with an accelerated decline in lung function and may be a contraindication to lung transplant
Respiratory
- Recurrent respiratory tract infections
- Bronchiectasis
- Respiratory failure in end stage disease
ENT
- Nasal polyps and recurrent sinusitis
Gastrointestinal
- Meconium ileus and rectal prolapse (neonate)
- Pancreatic insufficiency causing diabetes mellitus, enzyme insufficiency and malabsorption (with chronic diarrhoea)
- Gallstones
- DIOS (distal intestinal obstruction syndrome) this is the equivalent of meconium ileus in adults and involves blockage of the intestine due to thickened stool and sticky intestinal contents. It typically presents with fairly similar symptoms to small bowel obstruction including abdominal pain, reduced bowel movements and vomiting.
- CF related liver disease this may present as either a hepatic or a cholestatic picture. It results from plugging of liver bile ducts by dehydrated, viscous bile which can lead to focal liver damage. Repeated liver injury over time can cause these areas to become fibrosed and in some cases cirrhotic.
Other
- Failure to thrive (neonate)
- Osteoporosis and non-erosive arthropathy
- Subfertility/infertility in males this is due to defective sperm transport rather than abnormal spermatogenesis.
The median predicted survival for someone with cystic fibrosis currently stands at 41 years old.
In a respiratory station:
- CF patients are often caucasian, younger, have short stature and low BMI
- Clues around the bed: sputum pots, inhalers, nebuliser or NIV machines, physiotherapy devices, nutritional supplements and insulin pens
- May have a gastrostomy tube (abdomen)
- May have a long term vascular access (e.g. a portacath on the anterior chest wall or a PICC line in the ante-cubital fossa)
- May have clubbing
- Often will have coarse inspiratory creps on auscultation that might clear on coughing (consistent with bronchiectasis)
- May have a wheeze
- Screening at birth with the Guthrie heel prick test
- A sweat test is carried out in those presenting with CF symptoms a small sample of sweat is collected and a chloride level > 60mmol/L confirms the diagnosis
- Genetic analysis to screen for common mutations
Further investigations will then be carried out including
- Bloods including vitamin (A, E and D) levels plus aspergillus serology (20% develop ABPA - allergic bronchopulmonary aspergillosis)
- Annual oral glucose tolerance test to check for diabetes mellitus
- Annual liver function tests to screen for CF related liver disease
- Sputum samples for culture
- Chest radiographs to assess for infection or bronchiectasis
- Abdominal ultrasound may show fatty liver, cirrhosis or chronic pancreatitis
- Spirometry: this can show an obstructive deficit (FEV1/FVC <0.7)
The management of cystic fibrosis requires a multi-disciplinary team including respiratory physicians, specialist nurses, physiotherapists, occupational therapists, dieticians and psychologists.
Patient and family education about the condition itself is vital, and it is important to offer the patient or relative further information in the form of leaflets and links to the Cystic Fibrosis Trust UK (http://www.cysticfibrosis.org.uk/).
Optimization of nutrition is another important supportive measure:
- Regular input from a dietician many patients struggle to maintain weight especially if intercurrent infection
- Creon (enzyme replacement taken with meals)
- Fat soluble vitamin supplementation
- Oral nutritional supplements such as ensure/fortisip
- Some may require supplementary enteral feeding, often overnight via a PEG (Percutaneous endoscopic gastrostomy) or RIG (Radiologically Inserted Gastrostomy) though this is after careful assessment and discussion with a gastroenterology nutritional specialist
Psychological support is also vital. Cystic fibrosis is a lifelong, progressive condition. The burden of treatment is often significant and this can have a strong psychological input on both patients and their families. Adhering to strict treatment regimes which are disruptive to day to day life can be very difficult for patients.
Medical treatment is important to tackle the medical complications of cystic fibrosis, and the importance of compliance with treatment should be stressed for long term prognosis.
- Insulin for those who have pancreatic insufficiency and develop diabetes (oral hypoglycaemics are not effective in CF related diabetes)
- Prophylactic antibiotics which may be oral or nebulised (e.g. azithromycin or tobramycin)
- Vaccinations such as Pneumovax and HiB
- Bronchodilators (salbutamol) if any evidence of a reversible obstructive deficit on lung function tests
- Regular inhaled steroid to reduce airway inflammation this may be switched to oral or intravenous during exacerbations
- Hospital admission for prolonged courses of intravenous antibiotics is usually required for infective exacerbations (10-14 days)

- Daily chest physiotherapy/sputum clearance plus regular exercise
- This may involved postural drainage, chest percussion, controlled breathing exercises or forced expiration
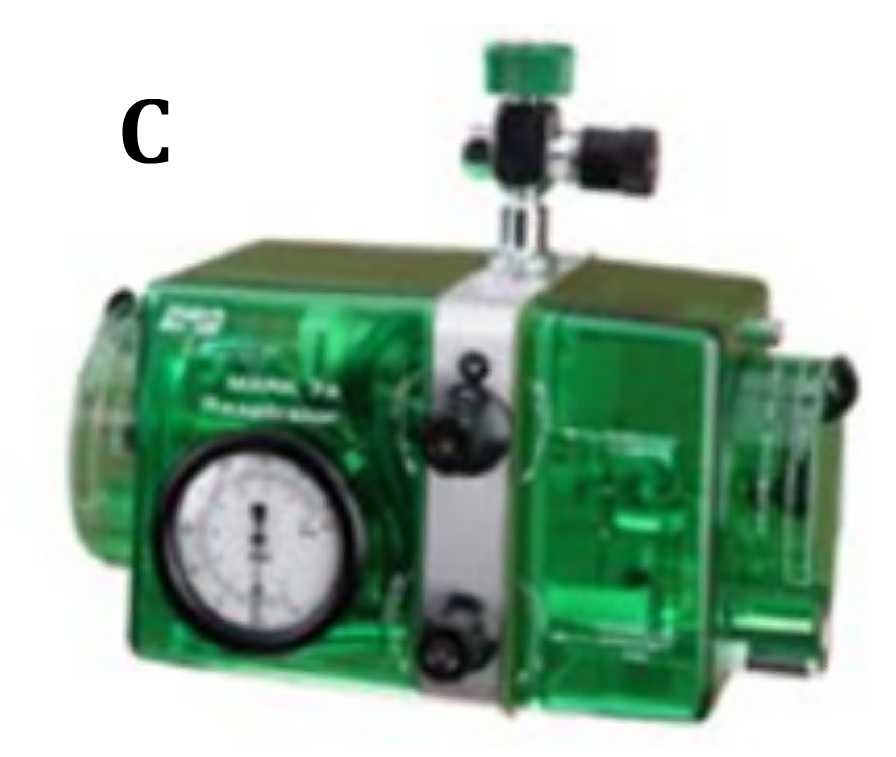
- A number of devices are available to help with physiotherapy. They work by generating PEEP (positive expiratory airways pressure) and therefore help with expectoration. They may be hand held (A and B) or may be larger pieces of equipment such as the bird (C). These help by generating positive pressure which help with sputum clearance and also support the patients work of breathing.
- Mucolytic medications such as oral carbocisteine or nebulised DNAse help to break down mucous and aid sputum clearance. Nebulised hypertonic saline or mannitol can also be trialled.
- In cases of DIOS (distal intestinal obstruction syndrome), high dose laxatives and/or enemas are necessary. Occasionally an NG (nasogastric) tube may also be needed either if vomiting is a predominant symptom or if the patient is not able to tolerate the large volumes of laxatives orally.
- In end stage disease, long term oxygen therapy and non invasive ventilation may be needed, under the close supervision of a respiratory physician.
- Gene therapy is now available for certain mutations however this should only be explored with CF specialists.

The mainstay of surgical intervention is bilateral lung transplantation. This offers a lot of hope to cystic fibrosis sufferers however is a major operation and therefore carries considerable risk. It is not an option for everybody and each patient has to be carefully assessed by a CF and transplant team before it is considered. This is an intensive and complex process.
It must also be remembered that transplant does not offer a complete cure it replaces the lungs but medications are still required for all other parts of the body that remain affected.
Unfortunately at present, there are many more patients that want/need a transplant than there are donor organs available.
first posted on: 15/02/2016; 12:37
